The 6 most common types of eating disorders and what to do: This post delves into the complexities of six prevalent eating disorders, from anorexia nervosa to binge eating disorder. We’ll explore the defining characteristics, potential health risks, and importantly, the available resources for support and recovery. Understanding these conditions is crucial for recognizing the signs and taking the first step towards seeking help.
Each disorder presents unique challenges, impacting individuals physically and mentally. This in-depth look at anorexia, bulimia, binge eating disorder, ARFID, and OSFED will equip you with essential knowledge. Furthermore, we’ll discuss effective treatment options and vital support systems. The journey to recovery is possible with the right guidance and resources.
Introduction to Eating Disorders
Eating disorders are serious mental illnesses characterized by a harmful relationship with food and body image. They profoundly impact an individual’s physical and emotional well-being, leading to a range of health complications and distress. These disorders are not simply about food; they are complex conditions rooted in a combination of biological, psychological, and social factors. Recognizing the signs and understanding the importance of seeking help is crucial in supporting those affected.These conditions aren’t about willpower or personal flaws.
They are medical conditions that require professional intervention and support. Early intervention and treatment can significantly improve outcomes, fostering recovery and a healthier relationship with food and body image. It’s essential to approach these issues with empathy, understanding, and a commitment to helping those struggling find the resources they need.
Prevalence of Eating Disorders
The prevalence of eating disorders varies across different demographics. Studies suggest that eating disorders are not limited to a specific group but can affect people of various ages, genders, ethnicities, and socioeconomic backgrounds. The incidence rate is relatively high in adolescents and young adults, often coinciding with significant life transitions and pressures.
- Adolescents and young adults often face increased pressure to conform to societal beauty standards and body ideals. This pressure, combined with hormonal changes and developmental stressors, can increase the risk of developing an eating disorder.
- Individuals from diverse backgrounds and experiences can be affected by eating disorders. Addressing these conditions requires a comprehensive understanding that considers various social, cultural, and economic influences.
- While specific statistics vary by region and study, the prevalence rates consistently highlight the importance of awareness and support for those affected.
Resources for Individuals with Eating Disorders
Accessing appropriate support is critical for individuals struggling with eating disorders and their families. A range of resources can provide guidance, treatment, and community support.
- National Eating Disorders Association (NEDA): Provides valuable information, support groups, and treatment referrals. Their website offers a wealth of resources for individuals, families, and professionals.
- National Association of Anorexia Nervosa and Associated Disorders (ANAD): This organization focuses specifically on anorexia nervosa and associated disorders. They offer educational materials, support groups, and information for individuals struggling with these conditions.
- Local mental health clinics and hospitals: Often offer specialized eating disorder programs and treatment options. Consult with healthcare providers to find suitable local resources.
- Support groups and online forums: These communities provide a space for sharing experiences and offering support to others facing similar challenges. However, it’s essential to ensure these resources are reputable and offer professional guidance.
Overview of Common Eating Disorders
Eating disorders encompass a variety of conditions, each with unique characteristics and impacts. Recognizing these differences is crucial for providing appropriate support and treatment.
- Anorexia nervosa: Characterized by a relentless pursuit of thinness, often leading to severe weight loss and distorted body image. It involves restrictive eating patterns, intense fear of gaining weight, and an overvaluation of body shape and weight.
- Bulimia nervosa: Involves cycles of binge eating followed by compensatory behaviors like purging (e.g., self-induced vomiting, laxative abuse) or excessive exercise. These behaviors aim to prevent weight gain and are driven by a strong fear of weight gain.
- Binge-eating disorder: Involves recurrent episodes of consuming large quantities of food in a short period, often accompanied by feelings of loss of control. Unlike bulimia, binge-eating disorder does not involve compensatory behaviors.
- Avoidant/Restrictive Food Intake Disorder (ARFID): Involves a persistent lack of interest in or avoidance of food, leading to nutritional deficiencies and potential health problems. This disorder can manifest in different ways, from extreme picky eating to complete aversion to certain food groups.
- Orthorexia nervosa: An obsession with healthy eating, often leading to extreme dietary restrictions that may cause significant health problems. Individuals with orthorexia may become fixated on specific food groups or preparation methods, potentially leading to nutritional deficiencies.
- Other Specified Feeding or Eating Disorders (OSFED): This category encompasses eating disorders that don’t fit neatly into the other categories but still cause significant distress and health problems. Examples might include disordered eating patterns or concerns about body shape or weight, but not meeting the full criteria for anorexia, bulimia, or binge-eating disorder.
Anorexia Nervosa
Anorexia nervosa is a serious eating disorder characterized by an intense fear of gaining weight and a distorted body image. Individuals with anorexia often have a significantly low body weight, and their perception of their body size is often inaccurate, leading to relentless efforts to maintain or achieve an abnormally low weight. This relentless pursuit of thinness can have devastating consequences on physical and mental health.
Key Characteristics
Anorexia nervosa is defined by a profound fear of gaining weight, even when underweight. This fear drives restrictive eating behaviors and often leads to a distorted body image, where individuals see themselves as significantly heavier than they actually are. This distorted perception is a crucial element in understanding the disorder. It’s not simply a matter of wanting to be thin; it’s a deeply ingrained and often unshakeable belief system.
Potential Medical Complications
The severe restriction of calories and nutrients in anorexia nervosa can lead to a multitude of medical complications. Electrolyte imbalances are a significant concern, potentially causing irregular heartbeats, muscle weakness, and even cardiac arrest. Osteoporosis, a condition characterized by weakened bones, is also a common consequence due to the lack of essential nutrients. Cardiovascular problems, such as heart failure and reduced heart rate, can develop as the body struggles to compensate for the lack of nourishment.
In severe cases, these complications can be life-threatening.
Subtypes of Anorexia Nervosa
Anorexia nervosa presents in different subtypes, each with its own behavioral patterns. The restricting type involves severe calorie restriction and avoidance of food, while the binge-purge type involves episodes of binge eating followed by compensatory behaviors like purging (e.g., vomiting, laxative use, or excessive exercise). Understanding these subtypes is essential for developing tailored treatment approaches. The binge-purge type often presents with more severe medical complications due to the added stress on the body from the binge-purge cycle.
Psychological Factors
Several psychological factors can contribute to the development of anorexia nervosa. These include low self-esteem, perfectionism, anxiety disorders, and a history of trauma or abuse. These factors can create a vulnerable environment where individuals turn to restrictive eating as a means of coping with emotional distress or seeking a sense of control over their lives.
Common Behaviors
Individuals with anorexia nervosa exhibit various behaviors aimed at controlling their weight and maintaining their low body weight. These behaviors often include severely restricting food intake, meticulously weighing and measuring food portions, exercising excessively, and engaging in purging behaviors like vomiting or using laxatives. The behaviors can become ritualistic and deeply ingrained, making it difficult to change them without professional intervention.
Symptoms of Anorexia Nervosa
| Symptom | Description | Severity Level | Treatment |
|---|---|---|---|
| Severely restricted eating | Significant reduction in food intake, often below minimum daily caloric needs. | Mild, Moderate, Severe | Nutritional counseling, meal planning, support groups |
| Distorted body image | An inaccurate perception of one’s body size and shape, often seeing oneself as overweight despite being underweight. | Mild, Moderate, Severe | Cognitive behavioral therapy (CBT), body image therapy |
| Excessive exercise | Intense physical activity beyond normal levels, often used as a means to burn calories and avoid weight gain. | Mild, Moderate, Severe | Physical therapy, exercise counseling, motivational interviewing |
| Purging behaviors | Engaging in behaviors like vomiting, laxative misuse, or diuretic abuse to compensate for perceived overeating. | Mild, Moderate, Severe | Medical intervention, psychotherapy, support groups |
| Amenorrhea | Absence of menstruation in females. | Moderate, Severe | Medical monitoring, hormone therapy |
Bulimia Nervosa
Bulimia nervosa is an eating disorder characterized by a cycle of binge eating followed by compensatory behaviors aimed at preventing weight gain. Individuals with bulimia often experience intense feelings of guilt, shame, and distress surrounding their eating habits, creating a cycle that can be incredibly difficult to break. Understanding the defining features, potential health risks, and contributing factors is crucial for recognizing and addressing this serious condition.Bulimia nervosa is marked by a relentless pursuit of thinness, often coupled with a distorted body image.
The intense fear of gaining weight, though often unrecognized by the individual, drives the compulsive behaviors associated with the disorder. The individual may not appear outwardly thin, as is often seen in anorexia nervosa, which can lead to a misdiagnosis or delayed intervention. This underscores the importance of recognizing the diverse presentations of eating disorders.
Defining Features, The 6 most common types of eating disorders and what to do
Bulimia nervosa is fundamentally defined by recurrent episodes of binge eating, followed by compensatory behaviors. Binge eating involves consuming a large quantity of food in a relatively short period, often feeling a lack of control over the eating. These episodes are frequently accompanied by feelings of guilt, shame, and distress. The compensatory behaviors that follow are designed to prevent weight gain, and can include self-induced vomiting, excessive exercise, misuse of laxatives, diuretics, or enemas, or fasting.
These compensatory behaviors are a crucial element in differentiating bulimia from other eating disorders.
Health Risks
Bulimia nervosa carries a significant risk of both immediate and long-term health complications. Dental problems, such as enamel erosion and tooth decay, are common due to the repeated exposure of teeth to stomach acid from induced vomiting. Electrolyte imbalances, including imbalances in potassium, sodium, and chloride, can result from purging behaviors, potentially leading to serious health issues such as heart problems, kidney damage, and even death.
The long-term effects on the cardiovascular system, digestive system, and overall well-being can be severe.
Psychological Factors
Several psychological factors can contribute to the development and maintenance of bulimia nervosa. These include low self-esteem, perfectionism, anxiety, depression, and a history of trauma or abuse. The feelings of inadequacy, guilt, and shame associated with binge-purge cycles often stem from underlying emotional issues. Furthermore, societal pressures to conform to idealized beauty standards and cultural norms surrounding body image can play a significant role.
Behaviors Associated with Bulimia Nervosa
Individuals with bulimia nervosa engage in a range of behaviors. These behaviors can include:
- Secretly eating large quantities of food in short periods of time.
- Engaging in compensatory behaviors to prevent weight gain, such as self-induced vomiting, misuse of laxatives or diuretics, excessive exercise, or fasting.
- Experiencing significant distress and shame regarding eating habits.
- Having a distorted body image and an intense fear of gaining weight.
- Engaging in frequent weighing and measuring of body size.
These behaviors are often performed in secret, compounding the sense of isolation and guilt associated with the disorder.
Comparison with Anorexia Nervosa
While both anorexia and bulimia nervosa involve disordered eating, they differ significantly in their presentation and consequences. Anorexia nervosa is primarily characterized by significantly low body weight, whereas bulimia nervosa does not necessarily involve such extreme weight loss. Furthermore, bulimia nervosa often involves binge eating and compensatory behaviors, while anorexia nervosa typically focuses on restriction and avoidance of food.
The underlying psychological factors and societal influences may also differ, although both conditions are rooted in a complex interplay of biological, psychological, and social factors.
Symptoms of Bulimia Nervosa
| Symptom | Description | Severity Level | Treatment |
|---|---|---|---|
| Binge Eating | Eating a large amount of food in a short period of time, feeling a lack of control. | Mild: Occasional episodes; Moderate: Frequent episodes; Severe: Daily or near-daily episodes. | Therapy, nutritional counseling, and potentially medication. |
| Compensatory Behaviors | Actions taken to prevent weight gain after binge eating, such as self-induced vomiting, misuse of laxatives, or excessive exercise. | Mild: Occasional use; Moderate: Frequent use; Severe: Daily or near-daily use. | Therapy, nutritional counseling, and potentially medication. |
| Distorted Body Image | An inaccurate perception of one’s body shape or size, often leading to an intense fear of gaining weight. | Mild: Some concern; Moderate: Significant concern; Severe: Extreme concern. | Therapy focused on body image and self-esteem, potentially in conjunction with medication. |
| Emotional Distress | Experiencing intense feelings of guilt, shame, anxiety, and depression related to eating habits. | Mild: Occasional feelings; Moderate: Frequent feelings; Severe: Persistent and overwhelming feelings. | Therapy focused on emotional regulation, potentially in conjunction with medication. |
This table Artikels the key symptoms of bulimia nervosa, categorized by their description, severity level, and potential treatment approaches. It is crucial to remember that this is not an exhaustive list, and individual experiences can vary significantly.
Understanding the six most common eating disorders and how to help is crucial. From anorexia nervosa to binge eating disorder, these conditions impact individuals in profound ways. Thankfully, there’s support available. Recent news about the ZTE trade ban lifted by the US Commerce Department under the Trump administration, while seemingly unrelated, highlights the complexities of global trade and its potential ripple effects.
Seeking professional help is vital for anyone struggling with an eating disorder, regardless of the current political landscape, and resources like the National Eating Disorders Association ( zte trade ban lifted us commerce department trump ) are invaluable. It’s important to remember that recovery is possible, and reaching out is the first step towards healing.
Binge Eating Disorder: The 6 Most Common Types Of Eating Disorders And What To Do
Binge eating disorder (BED) is a serious eating disorder characterized by recurrent episodes of binge eating, accompanied by feelings of distress and lack of control. Unlike bulimia nervosa, individuals with BED do not engage in compensatory behaviors to prevent weight gain. This lack of compensation can lead to significant weight gain and a host of related health problems.
Understanding the triggers and emotional underpinnings of BED is crucial for effective treatment and recovery.
Defining Features of Binge Eating Disorder
Binge eating disorder is defined by recurrent episodes of eating significantly more food in a short period than most people would eat under similar circumstances. These episodes are accompanied by feelings of a lack of control over eating. Crucially, individuals with BED do not engage in compensatory behaviors like purging, fasting, or excessive exercise. This distinguishes BED from bulimia nervosa.
Emotional and Psychological Impact
BED can have a profound emotional and psychological impact. Individuals experiencing BED often report feelings of shame, guilt, and distress after binge eating episodes. These feelings can contribute to low self-esteem, anxiety, and depression. The lack of control associated with BED can create a cycle of self-criticism and negative self-perception.
Physical Health Consequences
The consistent consumption of excessive amounts of food in binge eating episodes leads to significant weight gain and related health issues. This can include an increased risk of developing type 2 diabetes, high blood pressure, high cholesterol, and cardiovascular disease. Furthermore, the physical strain on the digestive system due to frequent overeating can contribute to various stomach and intestinal problems.
Weight gain can also impact self-image and body positivity, perpetuating the cycle of BED.
Triggers for Binge Eating Episodes
Various factors can trigger binge eating episodes. These can include stress, emotional distress, feelings of boredom, sadness, or even social situations. For example, experiencing a significant life event, such as the loss of a loved one, could trigger a binge eating episode. Sometimes, it’s a seemingly insignificant event, like feeling overwhelmed at work or encountering a personal conflict.
Understanding the six most common eating disorders and knowing what steps to take is crucial. Seeking professional help is vital, and exploring resources like helpful third-party apps, such as google now third party apps , can offer additional support and tools. Ultimately, remember that recovery is possible and there are many avenues for help in navigating these challenges.
Furthermore, triggers can be specific foods or cravings.
Difference Between BED and Bulimia Nervosa
The key difference between BED and bulimia nervosa lies in the presence or absence of compensatory behaviors. Individuals with bulimia nervosa engage in behaviors such as purging, fasting, or excessive exercise to prevent weight gain after binge eating. In contrast, individuals with BED do not engage in these compensatory behaviors. This difference in compensatory actions significantly impacts the long-term health implications.
Symptoms of Binge Eating Disorder
| Symptom | Description | Severity Level | Treatment |
|---|---|---|---|
| Recurrent episodes of binge eating | Eating significantly more food in a short period than most people would eat under similar circumstances, accompanied by a sense of lack of control. | Mild: Episodes occur a few times per week. Moderate: Episodes occur several times per week. Severe: Episodes occur daily or almost daily. | Therapy, such as Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT), can be effective. Medication may also be prescribed in some cases. |
| Feeling distressed or disgusted after binge eating | Experiencing feelings of shame, guilt, or self-loathing after binge eating episodes. | Mild: Experiencing feelings occasionally. Moderate: Feelings are more frequent. Severe: Feelings are almost constant. | Therapy focusing on emotional regulation and self-esteem building. |
| Feeling a lack of control over eating during episodes | Inability to stop eating even when full or when it’s physically uncomfortable. | Mild: Some sense of loss of control. Moderate: Significant loss of control. Severe: Complete lack of control. | Therapy focusing on developing coping mechanisms and strategies for managing cravings and urges. |
| Engaging in compensatory behaviors | (Not applicable to BED) Individuals with BED do not engage in behaviors like purging, fasting, or excessive exercise. | N/A | N/A |
Avoidant/Restrictive Food Intake Disorder (ARFID)
Avoidant/Restrictive Food Intake Disorder (ARFID) is a complex eating disorder characterized by difficulties with eating or consuming certain types of food. It differs significantly from other eating disorders like anorexia or bulimia, as it’s not primarily driven by a fear of weight gain or body image concerns. Instead, it centers on a range of factors related to the food itself, leading to restrictive eating habits that can impact physical and mental health.ARFID encompasses a broad spectrum of experiences, from mild avoidance of specific foods to a complete refusal to eat certain food groups or textures.
This avoidance can stem from various underlying issues, impacting not only nutritional intake but also emotional well-being and social interactions. Understanding the nuances of ARFID is crucial for recognizing and addressing this often overlooked eating disorder.
Key Characteristics of ARFID
ARFID is defined by a persistent lack of interest in eating or consuming certain foods. This can manifest as a range of behaviors, from selective eating to a complete aversion to certain food groups or textures. A key distinguishing factor is that the avoidance isn’t primarily motivated by a fear of weight gain or body image concerns, but rather by a range of sensory, emotional, and/or psychological factors.
Emotional and Psychological Impact of ARFID
The emotional and psychological impact of ARFID can be substantial. Individuals with ARFID may experience feelings of anxiety, distress, and even depression related to their eating habits. Social situations, particularly those involving mealtimes, can become stressful and isolating. The constant worry about food choices and potential reactions can negatively impact self-esteem and overall well-being.
Potential Causes of ARFID
The causes of ARFID are often multifaceted and involve a combination of environmental and psychological factors. Environmental factors might include negative experiences associated with certain foods, such as choking or vomiting incidents. Psychological factors might include sensory sensitivities, difficulties with sensory processing, or even past trauma that has created aversions to particular foods or eating situations. It’s important to note that ARFID can develop at any age and isn’t limited to specific demographic groups.
Understanding the 6 most common eating disorders and knowing what to do is crucial for support and recovery. While navigating these complex issues, consider the innovative features of Microsoft Teams, like the metaverse mesh and 3D avatars for meetings, which can help us connect and collaborate in new ways. Ultimately, seeking professional help and support remains the most effective way to address and overcome these disorders.
Medical Implications of ARFID
ARFID can lead to significant medical implications due to inadequate nutritional intake. Malnutrition can result in a variety of health problems, including growth retardation in children, anemia, and weakened immune systems. In severe cases, it can lead to serious health complications, impacting the overall quality of life. Long-term health consequences can arise from nutritional deficiencies, and early intervention is crucial for preventing complications.
Comparison to Other Eating Disorders
ARFID differs from other eating disorders like anorexia nervosa and bulimia nervosa in several key ways. Unlike anorexia and bulimia, which are primarily driven by body image concerns and weight control, ARFID is typically characterized by a lack of interest in consuming certain foods, often related to sensory issues, negative experiences, or psychological factors.
Symptoms of ARFID
| Symptom | Description | Severity Level | Treatment |
|---|---|---|---|
| Food Avoidance | Refusal to eat certain foods or food groups due to sensory issues, past experiences, or psychological factors. | Mild: Avoidance of a few foods; Moderate: Avoidance of several food groups; Severe: Avoidance of almost all foods. | Nutritional counseling, sensory integration therapy, addressing underlying psychological factors, and gradually introducing new foods. |
| Difficulty Eating | Experiencing discomfort or distress during mealtimes, or difficulty chewing and swallowing. | Mild: Discomfort during mealtimes; Moderate: Significant distress during meals; Severe: Complete refusal to eat. | Addressing sensory sensitivities, providing support during meals, and exploring underlying psychological factors. |
| Nutritional Deficiencies | Low intake of essential nutrients, resulting in symptoms like fatigue, weakness, and growth retardation (in children). | Mild: Minor deficiencies; Moderate: Significant deficiencies; Severe: Severe deficiencies requiring medical intervention. | Nutritional supplements, careful dietary planning, and possibly intravenous nutritional support. |
| Social Isolation | Avoiding social situations involving meals due to food restrictions. | Mild: Avoiding some social gatherings; Moderate: Avoiding most social situations; Severe: Complete isolation from social activities. | Social skills training, group therapy, and addressing underlying anxiety or social issues. |
Other Specified Feeding or Eating Disorders (OSFED)
Other Specified Feeding or Eating Disorders (OSFED) represent a diverse group of conditions that don’t quite fit neatly into the diagnostic categories of anorexia nervosa, bulimia nervosa, or binge-eating disorder. These individuals experience disordered eating patterns, but their symptoms don’t meet the full criteria for any of the established eating disorders. Understanding OSFED is crucial because it highlights the spectrum of eating-related challenges and the complexity of these conditions.
Defining Characteristics of OSFED
OSFED is characterized by persistent eating or related behaviors that cause significant distress or impairment in important areas of functioning. These behaviors deviate from typical eating patterns and are not adequately explained by another mental health condition. A key difference from other eating disorders lies in the absence of specific, defining features. Instead, OSFED captures the wide range of eating issues that don’t fit neatly into existing categories.
This variability is one of the significant challenges in diagnosis and treatment.
Examples of Conditions Falling Under OSFED
A wide array of conditions fall under the OSFED umbrella. These include individuals who experience episodes of binge eating but don’t exhibit compensatory behaviors like purging. They might also include individuals who restrict their food intake in a way that doesn’t meet the criteria for anorexia nervosa, or those who engage in disordered eating patterns related to specific life events or emotional distress.
It is important to remember that OSFED is not a catch-all category for all disordered eating behaviors. There is a need for a comprehensive assessment and a thorough evaluation to determine the precise nature of the eating problem.
Common Traits and Behaviors in OSFED
Individuals with OSFED often exhibit a range of common traits and behaviors. They might experience significant distress or concern about their body shape or weight, even if their weight is within a healthy range. They may also have difficulty controlling their eating, leading to irregular eating patterns and feelings of guilt or shame. Emotional distress and specific life events can often trigger these behaviors.
Comparing OSFED to Other Eating Disorders
OSFED differs from other eating disorders primarily in the lack of specific criteria. For example, individuals with anorexia nervosa exhibit significant weight loss, whereas those with OSFED might not. Individuals with bulimia nervosa regularly engage in compensatory behaviors (such as purging), which is not a characteristic of OSFED. Binge-eating disorder, while sharing the binge-eating component, differs in the absence of compensatory behaviors in OSFED.
The core distinction is the lack of specific features that define the other types of eating disorders.
Summary Table of OSFED
| Symptom | Description | Associated Traits | Treatment |
|---|---|---|---|
| Disordered eating patterns | Eating behaviors deviate from typical patterns, often with irregular mealtimes, skipping meals, or eating excessively at times. | Potential for emotional distress, feelings of guilt or shame, body image concerns. | Therapy, including cognitive behavioral therapy (CBT), interpersonal therapy (IPT), and nutritional counseling, tailored to address underlying issues and develop healthy eating habits. |
| Lack of specific criteria | Symptoms do not meet the criteria for other eating disorders. | Variable severity and presentation of symptoms. | Assessment by a qualified mental health professional is crucial to determine the appropriate course of action. |
| Significant distress or impairment | Disordered eating causes significant emotional distress or interferes with daily functioning. | Potential for comorbid conditions such as depression or anxiety. | Medical evaluation to rule out any underlying medical conditions. |
| Emotional triggers | Life events or emotional distress can trigger or exacerbate disordered eating behaviors. | May involve coping mechanisms that are maladaptive. | Focus on addressing the underlying emotional factors contributing to the disordered eating behaviors. |
Treatment and Support for Eating Disorders
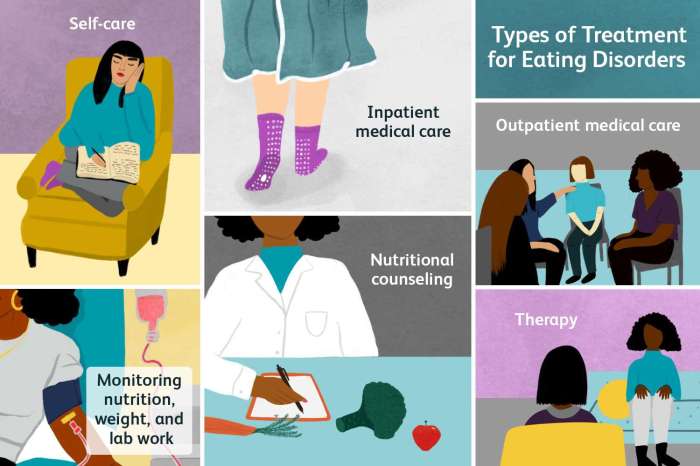
Recovering from an eating disorder is a challenging but achievable journey. It requires a comprehensive approach that addresses the physical, emotional, and psychological aspects of the illness. Successful treatment involves a strong support system, tailored interventions, and a commitment to long-term recovery. The road to recovery is unique to each individual, but understanding the various treatment options and support networks available can significantly enhance the chances of a positive outcome.Treatment for eating disorders is rarely a quick fix.
It’s a process that demands patience, self-compassion, and consistent effort from the individual, their family, and their support network. It necessitates a willingness to confront deeply ingrained behaviors and beliefs. The goal is not just to restore a healthy weight but to foster a healthier relationship with food and one’s body image.
Treatment Options
A multidisciplinary approach is crucial in the treatment of eating disorders. This means that a team of professionals, including therapists, doctors, dietitians, and psychiatrists, work collaboratively to create a personalized treatment plan. This collaborative effort ensures that all aspects of the individual’s well-being are addressed. This often includes a combination of therapies, nutritional counseling, and potentially, medication.
Importance of a Multidisciplinary Approach
A multidisciplinary approach ensures that all the relevant aspects of the eating disorder are addressed. A therapist can help identify underlying emotional issues and develop coping mechanisms. A doctor monitors physical health and can prescribe necessary medications. A dietitian provides guidance on healthy eating habits and nutritional needs. This holistic approach is essential because eating disorders often stem from a complex interplay of psychological, emotional, and physical factors.
Support Groups and Organizations
Finding support is vital for individuals struggling with eating disorders and their families. Numerous support groups and organizations offer valuable assistance. These groups provide a safe space for sharing experiences, offering encouragement, and learning coping strategies from others who understand. They also offer resources and information on the disorder, helping to alleviate feelings of isolation and providing practical support.
Examples include the National Eating Disorders Association (NEDA) and the National Association of Anorexia Nervosa and Associated Disorders (ANAD).
- The National Eating Disorders Association (NEDA) offers a helpline, support groups, and educational resources.
- The National Association of Anorexia Nervosa and Associated Disorders (ANAD) provides support and information specifically for those affected by anorexia nervosa and related disorders.
- Eating Disorders Anonymous is a fellowship of people who have or have had eating disorders.
Family Therapy
Family therapy plays a crucial role in the recovery process for individuals with eating disorders. It involves the family in the treatment, helping them understand the disorder and its impact on the individual and the family dynamic. This can lead to improved communication, reduced stress, and a more supportive environment for the individual to heal. Family therapy can also address the underlying family dynamics that may have contributed to the development of the eating disorder.
Types of Therapies
| Therapy Type | Description | Potential Benefits | Limitations |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | Focuses on identifying and changing negative thought patterns and behaviors related to food and body image. | Can help individuals challenge distorted thoughts, develop healthy coping mechanisms, and improve self-esteem. | May not be suitable for individuals with severe eating disorders or significant co-occurring mental health conditions. It can be demanding and require significant commitment. |
| Dialectical Behavior Therapy (DBT) | Teaches skills for emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness. | Can help individuals manage intense emotions, reduce impulsive behaviors, and improve relationships. | Can be time-consuming and requires significant effort. May not be suitable for everyone. |
| Family-Based Therapy (FBT) | Aimed at involving the family in the treatment process to promote healthy family communication and support. | Can create a supportive environment for the individual and foster healthy family dynamics. | Requires commitment from all family members. May not be appropriate for all families. |
| Interpersonal Therapy (IPT) | Focuses on improving interpersonal relationships and communication skills. | Can address social and relationship issues that may contribute to or exacerbate eating disorders. | May not be sufficient for individuals with severe underlying mental health conditions. |
Final Review
In conclusion, recognizing the signs and symptoms of eating disorders is the first step toward effective intervention. This exploration has highlighted the importance of seeking professional help and support for individuals struggling with these conditions. Remember, you are not alone, and recovery is possible. We hope this information empowers you to make informed decisions and take positive action.