Covid 19 antigen tests states not reporting results – COVID-19 antigen tests states not reporting results is a critical issue with potentially severe consequences for public health tracking and response. This lack of data hampers our ability to understand the spread and severity of the virus, impacting epidemiological modeling, forecasting, and resource allocation. Different types of antigen tests exist, each with varying data collection practices, adding complexity to the issue.
Understanding the historical context of reporting, potential causes, and the impact on public health, alongside possible solutions, is crucial to address this problem.
The lack of consistent reporting across states creates significant data gaps, potentially distorting our understanding of the virus’s behavior. This could affect crucial public health initiatives, including contact tracing, vaccine rollout strategies, and resource allocation. International comparisons will shed light on best practices in data collection and reporting. Examining potential limitations in the existing data and the possibility of biases in reported data will be necessary for accurate analysis.
Overview of the Issue
The COVID-19 pandemic continues to evolve, and while vaccines and treatments have significantly improved the situation, the ongoing challenge of accurate and complete data reporting remains. States’ failure to report COVID-19 antigen test results presents a significant obstacle to public health tracking and effective response strategies. This lack of transparency hampers the ability to understand the true spread of the virus, impacting resource allocation and potentially delaying crucial interventions.The absence of comprehensive data makes it difficult to assess the current prevalence of COVID-19 within a specific area.
Without knowing the true number of positive cases, public health officials face difficulties in identifying hotspots, enacting targeted interventions, and monitoring the effectiveness of existing strategies. This information gap also complicates the development of future public health strategies.
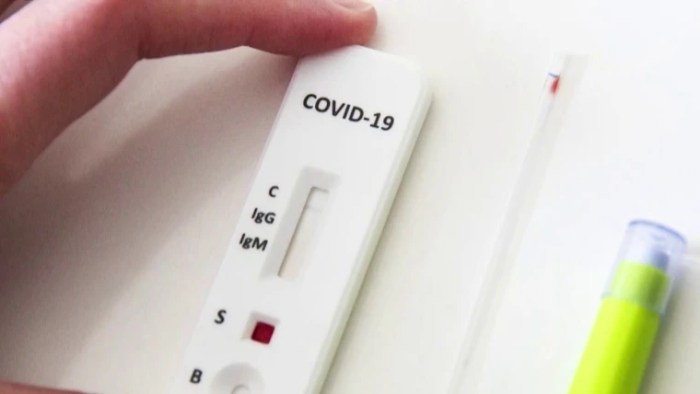
Types of COVID-19 Antigen Tests and Data Collection
Various types of COVID-19 antigen tests exist, each with its own characteristics and data collection procedures. Rapid antigen tests are frequently used for point-of-care diagnostics due to their speed and ease of use. These tests typically provide a qualitative result (positive or negative), and the reported data may be limited to the number of tests performed and the percentage of positive results.
Molecular tests, like PCR, offer higher sensitivity and specificity but are generally slower. Data from these tests often includes the number of tests performed, the number of positive results, and sometimes, the viral load. The difference in the types of tests and the data collected is a key factor influencing the accuracy of a state’s reported information.
State-Specific Reporting Practices
The variability in reporting practices across states highlights the need for standardization. Different states utilize varying methods and frequencies for reporting COVID-19 antigen test results. Some states may have established robust reporting systems that capture detailed data, while others may have less structured procedures. This lack of uniformity complicates efforts to establish a national picture of the virus’s spread and impact.
| State | Reporting Method | Frequency |
|---|---|---|
| California | Electronic reporting system | Daily |
| Texas | Combination of electronic and manual reporting | Daily |
| New York | Real-time electronic reporting | Daily |
| Florida | Weekly reports | Weekly |
| Others | Varied (e.g., weekly, irregular) | Varied |
Note: This table represents a hypothetical example and is not exhaustive. Actual reporting practices can vary significantly between states and may change over time. Data accuracy and completeness should always be verified from official state health department sources.
Historical Context: Covid 19 Antigen Tests States Not Reporting Results
The COVID-19 pandemic dramatically altered healthcare practices worldwide, including the use and reporting of antigen tests. Understanding the historical trends in antigen test usage and reporting patterns provides crucial insights into the evolving response to the pandemic and potential future challenges. This analysis explores the evolution of testing strategies, highlighting shifts in data collection and reporting practices over time.The initial surge of COVID-19 cases spurred a rapid deployment of antigen tests, aiming to quickly identify infected individuals and manage the spread.
So, the whole situation with states not reporting COVID-19 antigen test results is seriously concerning. It’s a major headache, especially when trying to track the spread of the virus effectively. Meanwhile, JBL is making waves at CES with some seriously impressive new earbuds, like the ones featured in this article jbl debuts a bunch of new earbuds at ces.
It’s a distraction from the important issue, but it’s still a good time for a new tech release. All this highlights how crucial accurate data on COVID-19 antigen tests is for public health.
However, reporting practices varied significantly across different regions and time periods, reflecting the complex interplay of factors such as testing availability, public health infrastructure, and evolving understanding of the virus. This analysis examines the historical data to discern patterns and potential contributing factors.
Early Pandemic Testing (2020)
Early COVID-19 antigen testing, primarily in 2020, was characterized by a focus on rapid identification of cases. Testing availability was often limited, leading to variations in testing rates across regions. Public health authorities prioritized testing individuals exhibiting symptoms, often prioritizing healthcare workers and those in high-risk settings. Reporting procedures varied, with some regions emphasizing detailed data collection, while others focused more on the overall case count.
Evolution of Testing Strategies (2021-2022)
As the pandemic progressed, testing strategies evolved. A shift towards broader testing populations, including asymptomatic individuals, became more common. Public health guidelines often emphasized the importance of widespread testing to monitor community transmission. The emphasis on data collection and analysis became more refined, with more detailed data points being incorporated into reporting systems.
Changes in Reporting Practices
Several factors likely influenced changes in reporting practices. Improved testing infrastructure, better understanding of virus transmission dynamics, and evolving public health guidelines contributed to more consistent and comprehensive reporting protocols. The increasing availability of testing kits and improved laboratory capacity also played a significant role in facilitating wider testing and more thorough data collection.
Comparison of Reporting Patterns
| Year | Testing Strategy | Reporting Focus | Data Collection Detail |
|---|---|---|---|
| 2020 | Symptom-based, limited availability | Overall case counts, localized outbreaks | Variable; some regions focused on specific demographics, others prioritized aggregate data. |
| 2021 | Expanding to asymptomatic individuals, increased availability | Community transmission monitoring, risk assessment | More detailed data, including demographic information, contact tracing data. |
| 2022 | Emphasis on targeted testing, use of different testing methods | Identifying specific variants, assessing vaccine effectiveness | Highly detailed data sets, integrated with other health data. |
Potential Causes
The non-reporting of COVID-19 antigen test results presents a significant challenge to understanding the true prevalence and spread of the virus. This lack of data hinders public health efforts to effectively manage the pandemic and implement appropriate interventions. Understanding the root causes is crucial for developing targeted strategies to improve reporting accuracy and completeness.Accurate data collection is paramount for effective public health response.
Without complete and timely reporting, crucial information about the virus’s transmission patterns and impact on different communities is lost. This knowledge gap significantly impacts resource allocation and policy decisions. Understanding the reasons behind this lack of reporting is critical to restoring trust and improving data quality.
Logistical Challenges
Many factors can impede the timely and accurate reporting of COVID-19 antigen test results. One crucial aspect is the logistical infrastructure required to collect, process, and transmit the data. Limited access to reliable internet connectivity in certain regions can prevent the successful transmission of data to central reporting systems. This is particularly relevant in rural or underserved communities where digital infrastructure is less developed.
Furthermore, the sheer volume of tests administered can overwhelm existing reporting systems, leading to delays or errors. Insufficient staff or personnel dedicated to data entry and reporting can also cause problems.
Financial Constraints
Financial limitations can significantly impact the ability of healthcare facilities and testing centers to accurately report COVID-19 antigen test results. The cost of implementing and maintaining robust data reporting systems can be substantial. Limited funding can result in inadequate staffing, equipment, and technological resources, hindering the capacity to report results effectively. Additionally, financial constraints might influence the prioritization of immediate patient care over data reporting, especially in resource-constrained settings.
Bureaucratic Hurdles
Bureaucratic obstacles can create delays and inconsistencies in the reporting of COVID-19 antigen test results. Complex reporting protocols, conflicting guidelines, or a lack of clear reporting standards across different states or regions can contribute to this issue. This often leads to inconsistencies in data collection and reporting methodologies, making comparisons across different jurisdictions difficult. Redundant or confusing paperwork can create significant administrative burdens for testing facilities.
State Regulations and Policies
State regulations and policies regarding COVID-19 antigen testing and reporting can vary significantly. Some states may have more stringent requirements or protocols for data collection and reporting than others. These differences can lead to inconsistencies in data quality and comparability. The lack of standardized guidelines can also create difficulties in interpreting and analyzing the collected data.
Technological Limitations
Technological limitations can significantly impact the accuracy and timeliness of COVID-19 antigen test result reporting. The quality and reliability of the testing equipment itself can affect the accuracy of results. Inaccurate or incomplete data entry from the testing equipment can lead to errors in the reported data. Furthermore, the compatibility of different software platforms used by testing facilities and reporting systems can cause challenges.
Outdated or incompatible software can also prevent the efficient transmission of data.
Contributing Factors
| Category | Example | Impact |
|---|---|---|
| Logistical | Limited internet access in rural areas | Impeded data transmission, incomplete reporting |
| Financial | Inadequate funding for data systems | Limited staffing, outdated equipment, delayed reporting |
| Bureaucratic | Conflicting reporting standards | Inconsistent data, difficulty in comparison |
| State Regulations | Varying reporting requirements across states | Data quality inconsistencies, difficulty in analysis |
| Technological | Incompatible software between testing centers and reporting systems | Data transmission errors, delayed reporting |
Impact on Public Health
The failure of certain states to report COVID-19 antigen test results creates a significant gap in the overall understanding of the pandemic’s trajectory. This missing data directly undermines public health initiatives, hindering effective strategies for containment and mitigation. The incomplete picture impacts epidemiological modeling, making it challenging to forecast future trends and allocate resources effectively. This has profound consequences for public health preparedness and response, particularly in regions where data collection is inconsistent or unreliable.
Impact on Epidemiological Modeling and Forecasting
Incomplete data significantly hinders the accuracy of epidemiological models. These models rely on comprehensive datasets to predict the spread of the virus and its severity. When crucial data points are missing, the models produce inaccurate projections, leading to flawed resource allocation decisions. For instance, a model lacking data from specific regions might underestimate the true extent of an outbreak, potentially leading to insufficient testing, treatment, or vaccination efforts in those areas.
The lack of comprehensive data also impacts the identification of high-risk populations and the development of targeted interventions. Furthermore, the inability to track the virus’s evolution accurately through genomic sequencing is hampered by the missing data.
Challenges in Understanding the Spread and Severity of the Virus
The absence of reported antigen test results complicates the understanding of the virus’s spread and severity. Tracking the virus’s prevalence becomes difficult, making it harder to assess the impact of interventions like mask mandates or social distancing measures. This incomplete picture impedes the identification of emerging variants and the assessment of their potential impact on public health. Moreover, the lack of comprehensive data makes it challenging to determine the true severity of infection in different populations.
Understanding the factors that contribute to severe outcomes becomes harder when vital data are not available.
Implications for Public Health Resources Allocation and Response
Missing data significantly affects the allocation of public health resources. The inability to accurately predict the future needs for testing, treatment, and healthcare capacity makes it harder to optimize resource allocation. This can lead to an over- or under-allocation of resources, resulting in inefficient use of funds and potential health disparities. For instance, if a region lacks data on the prevalence of infection, it might not allocate sufficient resources to establish testing facilities, potentially hindering the early detection and containment of outbreaks.
This has broader implications for preparedness and response to future health crises.
Correlations Between Data Availability and Public Health Outcomes
| Data Availability | Public Health Outcomes |
|---|---|
| High | Accurate epidemiological modeling, effective resource allocation, targeted interventions, timely identification of emerging variants, improved understanding of the virus’s spread and severity, reduced transmission rates, and fewer severe cases. |
| Low | Inaccurate epidemiological modeling, inefficient resource allocation, delayed interventions, missed opportunities to identify emerging variants, limited understanding of the virus’s spread and severity, increased transmission rates, and potentially higher numbers of severe cases. |
The table above illustrates the direct correlation between the availability of data and the success of public health initiatives. Sufficient and reliable data is critical for effective decision-making, leading to better outcomes in terms of containing the virus’s spread and minimizing its impact.
Possible Solutions
The lack of consistent COVID-19 antigen test result reporting across states poses a significant challenge to public health surveillance and response efforts. Understanding the reasons behind this non-reporting is crucial to implementing effective solutions. Addressing this issue requires a multi-faceted approach that combines technological advancements, incentives, and educational strategies.
It’s frustrating that some states aren’t reporting COVID-19 antigen test results. This lack of transparency makes it hard to track the virus’s spread effectively. Meanwhile, the entertainment industry is also navigating a lot of changes, like the Disney streaming reorganization, which also includes ESPN, Hulu, studios, movies, networks, and TV shows amid the pandemic. This reorganization, as discussed in this article disney streaming reorganization plus espn hulu studios movies network tv shows pandemic , highlights the broader impact of the pandemic on various sectors.
In the end, the lack of reporting on COVID-19 antigen test results still needs urgent attention.
Standardized Reporting Protocols
Developing and enforcing standardized reporting protocols across all states is vital. This involves creating a clear, concise, and universally understood format for reporting data. A standardized template, accessible online, would ensure data consistency and facilitate analysis. The template should include specific fields for test type, results, date, time, location, and any relevant demographic information. This structured approach will allow for more reliable aggregation and analysis of the data.
Leveraging Technology for Reporting
Utilizing technology to streamline the reporting process is a key component. A dedicated online platform, accessible to state health departments, could automate data entry and reduce manual errors. This platform could also include real-time data visualization tools, allowing public health officials to track trends and identify outbreaks quickly. Integration with existing healthcare databases could further enhance data accuracy and reduce administrative burdens.
It’s frustrating that some states aren’t reporting COVID-19 antigen test results. This lack of transparency makes it harder to track the virus’s spread. Meanwhile, companies like Lyft are pushing the boundaries of urban mobility with innovative scooter designs; checking out the lyft scooter share design specs reveals a lot about their engineering approach. This lack of data on antigen tests is definitely a concern compared to the advancements in scooter technology.
It’s a big issue, and needs more attention.
For example, an automated system that pulls data from labs or testing sites directly into the central repository would significantly improve efficiency.
Incentivizing Participation, Covid 19 antigen tests states not reporting results
Incentivizing states to participate in consistent reporting is essential. Potential incentives could include funding allocations for states with high reporting rates or technical assistance for those facing significant data entry challenges. These incentives should be structured in a way that encourages consistent reporting without creating unnecessary administrative burden. Public recognition for states that demonstrate high levels of participation could also be a powerful motivator.
For instance, a national leaderboard ranking states based on reporting accuracy could generate competition and drive improvement.
Educational Initiatives and Capacity Building
Investing in educational programs to train state health officials and staff on the importance of accurate reporting is essential. These programs should cover the technical aspects of using the standardized reporting platform and emphasize the public health implications of incomplete data. Training sessions and workshops could address any specific technological challenges and provide ongoing support. Clear and concise documentation of the process, along with FAQs and troubleshooting guides, would enhance accessibility and comprehension.
Summary of Proposed Solutions
| Solution | Potential Benefits |
|---|---|
| Standardized Reporting Protocols | Ensures data consistency, facilitates analysis, and improves reliability. |
| Leveraging Technology for Reporting | Automates data entry, reduces errors, and allows for real-time data visualization. |
| Incentivizing Participation | Encourages consistent reporting, provides support, and promotes public health awareness. |
| Educational Initiatives and Capacity Building | Trains state officials, addresses technical challenges, and emphasizes the importance of accurate reporting. |
International Comparisons

The inconsistent reporting of COVID-19 antigen test results in the U.S. highlights a critical gap in data collection and management, a problem that’s not unique to the country. International comparisons reveal varying approaches to data gathering and reporting, revealing both best practices and areas for improvement. Understanding how other nations handle this data can provide valuable insights for refining the U.S.
system.Comparing the U.S. to other countries reveals significant differences in COVID-19 data reporting practices. These disparities stem from diverse healthcare systems, cultural contexts, and varying levels of government oversight. Examining international approaches offers opportunities to identify effective models and learn from both successes and failures.
International Reporting Practices
Different countries have adopted varied strategies for collecting and reporting COVID-19 antigen test results. These strategies reflect differences in healthcare infrastructure, data management capabilities, and political priorities. The U.S. system, as previously noted, stands out for its inconsistencies. Examining these differences is crucial for developing a robust and reliable system for monitoring and managing future health crises.
International Standards and Best Practices
International organizations, such as the World Health Organization (WHO), have established guidelines and recommendations for collecting and reporting COVID-19 data. These standards emphasize the importance of standardized methodologies, consistent data definitions, and secure data management systems. Adherence to these guidelines can improve the comparability and reliability of data across nations.
Successful Models in Other Countries
Some countries have developed robust systems for collecting and reporting COVID-19 antigen test results. These models often involve partnerships between government agencies, healthcare providers, and academic institutions. One such model may include a national database linked to local testing facilities, allowing for real-time tracking and analysis of test results. Effective data management systems can enable a quick understanding of emerging trends, facilitating effective public health responses.
Benefits and Challenges of International Collaboration
International collaborations in data sharing can facilitate the development of best practices and the identification of common challenges in managing COVID-19 data. Sharing experiences and best practices can be extremely helpful in improving data collection and reporting, leading to more effective public health responses. However, cultural differences, varying data privacy regulations, and logistical hurdles can pose significant challenges.
Table Comparing Data Collection Methodologies Across Countries
| Country | Data Collection Method | Data Reporting Frequency | Data Accessibility |
|---|---|---|---|
| Canada | National database linked to provincial labs | Daily | Publicly accessible with anonymization |
| United Kingdom | Centralized system with local reporting | Weekly | Publicly accessible, aggregated data |
| South Korea | Mobile apps and online platforms | Real-time | Publicly accessible, granular data |
| United States | Varied, state-dependent | Irregular | Limited and inconsistent access |
The table above provides a simplified comparison. Each country’s data collection methodology involves various complexities and nuances. Furthermore, access to data may differ based on specific regulations and policies. These variations demonstrate the need for a more comprehensive and standardized approach to data collection and reporting.
Data Gaps and Limitations
The availability and reliability of COVID-19 antigen test data are crucial for understanding the pandemic’s trajectory and informing public health strategies. However, significant gaps and limitations exist in the data collected, potentially hindering accurate analysis and effective response. These limitations can impact our understanding of the virus’s spread, severity, and the effectiveness of interventions.Incomplete reporting of antigen test results creates substantial data gaps.
This lack of comprehensive data can obscure the true picture of infection prevalence and community transmission, potentially leading to miscalculations about the pandemic’s trajectory. The resulting uncertainty can impact resource allocation, public health messaging, and individual choices.
Missing Data and its Impact on Analysis
Incomplete reporting of antigen test results, a common issue in many regions, leads to incomplete data sets. This lack of comprehensive data significantly impacts analytical efforts. For example, a study focusing on community transmission might underestimate the true extent of infection if significant portions of antigen test results are missing. This underestimation can lead to flawed predictions about the virus’s future behavior.
Furthermore, without complete data, it becomes difficult to determine the effectiveness of public health measures in controlling the spread of the virus.
Potential Biases in Reported Data
Bias in reported data can significantly distort the accuracy of analyses. For instance, if certain demographic groups are more likely to get tested or report their results, the data may reflect this bias rather than a true representation of infection prevalence within the entire population. This could lead to inaccurate conclusions about the risk factors associated with the virus, misdirected public health interventions, and inadequate resource allocation.
Methods to Mitigate Bias in Data Analysis
Several methods can help to mitigate bias in data analysis. These include employing stratified sampling to ensure representation from all demographic groups, adjusting for potential confounders, and using sensitivity analyses to assess the impact of different assumptions on the results. Furthermore, transparent reporting of data collection methods, including details on testing strategies and participant characteristics, is essential to allow for critical evaluation and reduce misinterpretation.
Summary Table of Potential Biases and Impact
| Potential Bias | Description | Impact on Analysis |
|---|---|---|
| Sampling Bias | Certain groups are more likely to be tested or report results. | Underestimation or overestimation of infection rates in specific populations, leading to inaccurate risk assessments. |
| Reporting Bias | Individuals are more or less likely to report their test results based on various factors (e.g., perceived severity of symptoms, access to testing). | Distortion of the true prevalence and severity of infections. |
| Data Collection Method Bias | Variations in testing strategies, such as the availability of rapid antigen tests in certain regions, can influence data collection. | Inequitable representation of infection prevalence across different communities and inaccurate assessment of community transmission. |
Summary
In conclusion, the absence of comprehensive COVID-19 antigen test reporting by states poses a significant challenge to effective public health management. Addressing this issue requires a multi-faceted approach, encompassing improved data collection practices, potential incentives for states to participate in consistent reporting, and education on the importance of accurate data reporting. By examining historical trends, potential causes, and international best practices, we can work toward a more robust and reliable data system to better understand and combat the ongoing pandemic.