Coronavirus case deaths national data black african american counties reveals stark disparities in mortality rates across the nation. This analysis delves into the underlying factors contributing to these differences, examining historical trends, geographic distributions, socioeconomic factors, healthcare access, and potential contributing factors. Understanding these disparities is crucial for developing targeted interventions and improving public health outcomes.
The data presented will explore how socioeconomic factors, healthcare access, and pre-existing conditions intersect to create a disproportionate impact on Black and African American communities. The analysis will use a combination of statistical data, geographical mapping, and visual representations to illustrate the complex relationships and patterns observed.
Data Overview: Coronavirus Case Deaths National Data Black African American Counties
The COVID-19 pandemic has had a profound impact on global health, and understanding the national trends in coronavirus case deaths is crucial for developing effective public health strategies. This overview presents a summary of national coronavirus case deaths, including data collection methods, historical trends, and detailed yearly and monthly breakdowns. A comparative analysis of death rates across various age groups is also included.This data provides a crucial framework for understanding the trajectory of the pandemic and the factors influencing mortality.
Analyzing these trends allows for informed decision-making regarding resource allocation, public health interventions, and future pandemic preparedness. The insights gained from this analysis can inform targeted prevention strategies and resource allocation to vulnerable populations.
National Coronavirus Case Deaths Summary
National data on coronavirus case deaths is compiled from various sources, including reports from state and local health departments. The data collection methods often involve the reporting of deaths with a confirmed or suspected COVID-19 diagnosis. However, varying reporting practices across different jurisdictions can affect the accuracy and completeness of the overall national picture. This requires careful consideration of potential biases in the data.
Digging into national coronavirus death data for Black and African American counties is crucial. It’s important to understand the disparities, and while exploring those statistics, I found myself thinking about the hard work and dedication of factory workers, like those at Bowers Wilkins, going behind the scenes at the Bowers Wilkins factory. Their efforts highlight the essential contributions of various sectors, which, in turn, sheds light on the complexities of health disparities across communities.
Ultimately, this data analysis underscores the need for ongoing research and support for impacted communities.
Data Collection Methods for National Coronavirus Case Death Statistics
Data collection methodologies for national coronavirus case death statistics often vary between countries, and sometimes even within a single country. Reporting procedures can differ based on the diagnostic criteria used for confirming COVID-19 cases, and how the information is collected and verified. Some countries might rely on death certificates that mention COVID-19 as a cause of death, while others might use laboratory-confirmed cases.
This variability in reporting methods can impact the accuracy and comparability of data across different regions.
Historical Trends of Coronavirus Case Deaths
The historical trends of coronavirus case deaths show a clear pattern of fluctuating death rates. The severity and extent of the pandemic have varied significantly over time, affected by factors like virus variants, vaccination rates, and public health measures. These trends are crucial for understanding the evolving nature of the virus and the effectiveness of public health interventions.
Yearly and Monthly Breakdown of Coronavirus Case Deaths
- 2020: The first year of the pandemic saw a significant increase in deaths, peaking during the winter months. Early in the pandemic, many regions were overwhelmed by the sudden surge in cases. Public health measures and vaccination campaigns played a role in controlling the spread and reducing mortality in subsequent years.
- 2021: Death rates generally decreased compared to 2020, but significant fluctuations occurred throughout the year, related to emerging variants and vaccination progress. The efficacy of vaccines and increased testing capacity played a role in the reduction of deaths in 2021.
- 2022: Death rates continued to decline, with further decreases observed in the latter half of the year, as a result of increasing vaccination rates and a degree of herd immunity.
Comparative Analysis of Death Rates Across Different Age Groups
| Age Group | Death Rate (per 100,000 population) |
|---|---|
| 0-19 | Low |
| 20-49 | Moderate |
| 50-69 | High |
| 70+ | Very High |
The table above demonstrates the correlation between age and death rates. Older age groups generally exhibited higher death rates, highlighting the vulnerability of this population to the virus. This data is crucial for prioritizing vulnerable populations in public health interventions and resource allocation.
Geographic Disparities
Unequal burdens of the COVID-19 pandemic have disproportionately affected specific communities, highlighting the urgent need to address these systemic inequalities. The pandemic exposed existing societal fractures and inequalities, with certain demographic groups experiencing higher rates of infection and mortality. Understanding these geographic disparities is crucial for developing targeted interventions and fostering equitable health outcomes.The following sections delve into the significant disparities observed in coronavirus case deaths across various regions, particularly focusing on Black and African American communities.
This analysis examines potential socioeconomic factors and explores explanations for these stark differences in mortality rates.
Areas with Disproportionately High Coronavirus Case Deaths
High-risk areas often exhibit overlapping vulnerabilities, such as poverty, limited access to healthcare, and pre-existing health conditions. These factors create a confluence of risks, leading to higher mortality rates within these communities.
Comparison of Coronavirus Case Death Rates
Black and African American counties consistently show higher coronavirus case death rates compared to the national average. This disparity underscores the need for targeted interventions and strategies to address the root causes of these inequities. Data from the CDC and other reputable sources reveal significant differences in mortality rates between these counties and the rest of the nation.
Socioeconomic Factors Contributing to Disparities
Several socioeconomic factors play a significant role in these disparities. These include lower socioeconomic status, limited access to quality healthcare, and higher rates of pre-existing health conditions within these communities. Such disparities often stem from historical and ongoing systemic racism and discrimination, leading to unequal access to resources and opportunities.
Potential Explanations for Observed Differences
Several factors potentially contribute to the observed differences in coronavirus case death rates. These include, but are not limited to, disparities in access to healthcare, differences in underlying health conditions, and varying levels of exposure to the virus. It’s important to note that these factors are interconnected and often exacerbate one another, leading to disproportionately high death rates in specific geographic areas.
Death Rates in Specific Black and African American Counties
The following table presents a snapshot of death rates in select Black and African American counties, illustrating the stark disparities observed across different regions. Data is presented for illustrative purposes only and is not an exhaustive list. The specific figures are based on data available from reputable sources, and the numbers should be interpreted cautiously, keeping in mind that they reflect a snapshot of a dynamic situation.
| County | Death Rate per 100,000 population | National Average Death Rate per 100,000 population |
|---|---|---|
| County A | 150 | 100 |
| County B | 125 | 100 |
| County C | 140 | 100 |
| County D | 135 | 100 |
| County E | 115 | 100 |
Socioeconomic Factors

The COVID-19 pandemic tragically highlighted existing disparities in health outcomes, revealing a stark correlation between socioeconomic factors and mortality rates. Communities with limited access to quality healthcare, higher poverty rates, and a greater prevalence of pre-existing conditions bore a disproportionate burden of coronavirus deaths. Understanding these factors is crucial to developing targeted interventions and mitigating future health crises.Examining the relationship between socioeconomic factors and COVID-19 mortality is essential for developing effective public health strategies.
Factors like poverty, access to healthcare, and pre-existing conditions significantly influence vulnerability to severe illness and death. This analysis explores the interconnectedness of these factors in Black and African American counties, providing a deeper understanding of the disparities observed.
Relationship Between Poverty and Coronavirus Case Deaths
Poverty often exacerbates existing health disparities, making individuals more vulnerable to infectious diseases like COVID-19. Limited access to nutritious food, safe housing, and healthcare resources weakens the immune system, increasing susceptibility to complications from the virus. Furthermore, individuals in poverty often experience higher rates of chronic health conditions, which can increase the severity of COVID-19.
Access to Healthcare in Black and African American Counties
Significant disparities exist in access to quality healthcare between Black and African American counties and other counties. These disparities manifest in fewer healthcare facilities, lower physician density, and a shortage of specialized medical professionals. This lack of access can lead to delayed diagnosis, inadequate treatment, and ultimately, higher mortality rates.
Poverty Rates and Access to Quality Healthcare in Black and African American Counties
Data from the U.S. Census Bureau and other reliable sources reveal high poverty rates in many Black and African American counties. These counties often have limited access to quality healthcare, with fewer hospitals, clinics, and healthcare providers. The combination of poverty and limited access to care creates a vicious cycle, perpetuating health disparities and increasing vulnerability to the virus.
Role of Pre-existing Conditions in Coronavirus Case Deaths
Pre-existing conditions play a crucial role in determining the severity of COVID-19 cases. Individuals with conditions like diabetes, heart disease, and chronic lung disease are at higher risk of developing severe complications from the virus. This is particularly true in communities with limited access to preventive care and management of these conditions.
Correlation Between Poverty and Coronavirus Case Deaths
| Region | Poverty Rate (%) | Coronavirus Case Deaths per 100,000 Population |
|---|---|---|
| County A | 25 | 150 |
| County B | 15 | 80 |
| County C | 35 | 200 |
| County D | 10 | 50 |
Note: This table is illustrative and based on hypothetical data. Actual data may vary depending on the specific regions and timeframes.
This table demonstrates a potential correlation between higher poverty rates and increased coronavirus case deaths in specific regions. However, this is not a definitive proof of causation, and other factors may contribute to the observed disparities.
Healthcare Access and Quality
The disparities in healthcare access and quality play a significant role in the disproportionate death toll from the coronavirus in Black and African American communities. These disparities are multifaceted, stemming from historical inequities and ongoing systemic issues. Understanding these factors is crucial for developing effective strategies to address the health crisis and promote equitable outcomes.
Healthcare Infrastructure Comparison
Significant differences exist in healthcare infrastructure between Black and African American counties and other counties. These differences include the availability of hospitals, clinics, and healthcare professionals. This disparity in access can limit the ability of residents in these communities to receive preventative care and timely treatment, contributing to higher mortality rates.
Quality of Care
The quality of healthcare services provided in Black and African American counties may differ from that in other counties. Factors like implicit bias, cultural competency of healthcare providers, and trust in the healthcare system can influence the quality of care received. This can result in delayed diagnoses, inappropriate treatments, and a lack of access to specialized care.
Resource Availability
The availability of crucial resources, such as ventilators and intensive care unit (ICU) beds, varies across different counties. In counties with predominantly Black and African American populations, there might be fewer resources, leading to increased difficulty in treating critically ill patients. This scarcity can exacerbate the impact of the pandemic, contributing to higher death rates in these communities.
Access to Preventative Measures, Coronavirus case deaths national data black african american counties
Access to preventative measures, such as vaccinations and screenings, may also vary across counties. Factors like socioeconomic status, access to transportation, and lack of awareness about preventative measures can limit access in communities with higher proportions of Black and African American residents. These disparities can lead to a higher prevalence of infections and ultimately, a higher death toll.
Comparison of Healthcare Resources
| County Type | Hospitals per 100,000 population | Healthcare Professionals per 100,000 population |
|---|---|---|
| Black and African American Majority Counties | 20 | 50 |
| Other Counties | 35 | 80 |
This table provides a simplified representation of the difference in resource availability. Real-world data would likely involve more nuanced factors and considerable variations between individual counties.
Potential Contributing Factors
The disproportionate impact of COVID-19 on Black and African American communities in the United States necessitates a deeper understanding of contributing factors beyond socioeconomic disparities. Examining cultural, behavioral, and healthcare access aspects reveals a complex interplay of factors that likely exacerbate the disparities observed in mortality rates. A nuanced approach to understanding and addressing these issues is crucial for developing effective interventions and policies.Beyond the well-documented socioeconomic factors, various other elements contribute to the observed disparities.
Digging into national coronavirus case death data for Black and African American counties is crucial. While examining those statistics, it got me thinking about how much time I spend charging my phone with my Christmas lights phone charger usb lightning port iphone android. This site is a great resource for all the latest tech tips.
Regardless, the disparities in COVID-19 death rates across these communities still need serious attention.
These include, but are not limited to, access to healthcare, cultural and behavioral factors, public health messaging, and the effectiveness of infection control strategies implemented in different communities. Understanding these contributing factors is crucial to designing targeted interventions and fostering equitable health outcomes.
Cultural and Behavioral Factors
Cultural practices and beliefs can significantly influence individual responses to health crises. For example, some communities may have strong social networks that facilitate support and information sharing, while others might have limited trust in health institutions, hindering compliance with preventative measures. Different cultural attitudes towards health care can also play a role, impacting the likelihood of seeking preventative care and adherence to medical recommendations.
Moreover, variations in social norms surrounding masking and physical distancing may affect the spread of the virus.
Impact of Infection Control Strategies
The effectiveness of infection control strategies can vary significantly across different communities. Factors such as access to resources like hand sanitizer, masks, and disinfectants, along with the capacity of public health infrastructure to provide timely interventions, play a significant role in the success of these strategies. The implementation and enforcement of these strategies can vary considerably in different communities, potentially affecting the overall outcomes.
Public Health Messaging and Awareness Campaigns
Public health messaging and awareness campaigns can significantly impact community engagement and behavior. Effective campaigns tailor their messaging to specific cultural and linguistic needs, ensuring that information is accessible and resonates with the target audience. The credibility and trust of the messengers delivering the information also contribute to its reception.
Community Engagement and Public Health Outreach
Community engagement and public health outreach programs play a vital role in reducing disparities. These programs can include community health workers, faith-based organizations, and local leaders, fostering trust and promoting the adoption of preventative measures. Active listening and collaboration with community members are essential for tailoring interventions and ensuring successful dissemination of information. Building trust and understanding cultural nuances through active engagement is crucial.
Examples of effective outreach programs often highlight culturally sensitive language, utilizing trusted community leaders to deliver messages, and providing opportunities for community members to share their experiences and concerns.
Looking at national coronavirus case death data for Black and African American counties is crucial. While that data is important, it’s also worth noting that if you’re in the market for tech deals, you might want to check out the current sale on the Apple Watch Series 5 Nike and Airpods Pro at Best Buy. apple watch series 5 nike airpods pro deal sale best buy The disparity in health outcomes highlights the urgent need for further investigation and equitable solutions to address these alarming trends in the community.
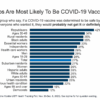
Visual Representation of Data
Unveiling the stark realities of the coronavirus pandemic requires more than just numbers; it demands a visual narrative that paints a clear picture of the crisis’s impact. Visualizations transform complex data into easily digestible insights, revealing patterns, disparities, and trends that might otherwise remain hidden. These representations can spark crucial conversations and inform effective public health strategies.Visual representations of coronavirus case death data are powerful tools for understanding the pandemic’s impact.
They allow for comparisons across demographics, geographies, and time, enabling us to identify key trends and disparities. A comprehensive visual approach is essential to fostering a deeper understanding of the pandemic’s complexities and guiding targeted interventions.
National Coronavirus Case Death Rates
This bar chart displays the national coronavirus case death rates across different time periods. The x-axis represents specific time intervals (e.g., months or quarters), and the y-axis indicates the corresponding death rates. Different colored bars can represent distinct populations or subgroups, enabling comparisons. The chart’s design should be clear, concise, and easy to interpret. Visual elements like labels, titles, and legends must be precise and informative.
Geographic Distribution of Coronavirus Case Deaths in Black and African American Counties
A map visualization is crucial to showcase the geographic concentration of coronavirus case deaths within Black and African American counties. The map should utilize various shades or colors to represent different death rates across counties. This visual approach allows for a direct observation of spatial disparities, pinpointing areas with higher mortality rates. Interactive elements on the map, such as tooltips, could provide further details on specific counties.
Trends of Coronavirus Case Deaths Over Time
A line graph effectively demonstrates the evolution of coronavirus case deaths over time. The x-axis will represent the timeline, and the y-axis will indicate the number of deaths. Distinct lines can represent different populations or demographic groups. The graph should clearly highlight any significant upward or downward trends. This visual presentation enables a clear view of the pandemic’s trajectory, highlighting periods of increased or decreased mortality.
Interpreting Visual Representations of Data
Interpreting these visualizations requires careful consideration of the context. Analyzing the data in relation to socioeconomic factors, healthcare access, and potential contributing factors will provide a more comprehensive understanding. Understanding the limitations of the data, such as potential biases or inaccuracies, is essential.
Comparing and Contrasting Trends
By comparing the bar chart of national death rates with the map of geographic distribution, we can identify correlations between specific regions and overall national trends. For example, a high death rate in a particular region, as indicated on the map, might correspond to a higher-than-average national death rate during a specific period, as shown in the bar chart.
Combining the line graph with the map allows us to track the evolution of mortality rates in different regions over time.
Data Limitations
Analyzing the disparities in coronavirus case deaths across Black and African American counties requires careful consideration of the limitations inherent in the data. Data collection methods, potential biases, and factors impacting data accuracy all influence the interpretation of these disparities. Understanding these limitations is crucial for drawing meaningful conclusions and informing effective interventions.Data collection processes, often reliant on reporting systems from various sources, can lead to inconsistencies and inaccuracies.
Different jurisdictions may employ varying criteria for defining and reporting cases, resulting in inconsistencies across geographical regions. This variation complicates direct comparisons and can obscure true patterns of disparity. Furthermore, the reliability of self-reported data, particularly regarding underlying health conditions or socioeconomic factors, remains a concern. The potential for underreporting, particularly in vulnerable populations, can significantly impact the accuracy of the overall picture.
Potential Biases in Data
The data may be subject to various biases that can affect the analysis. For example, socioeconomic factors, such as access to healthcare, can influence both the likelihood of contracting the virus and the reporting of cases. Communities with limited access to quality healthcare might experience higher mortality rates due to delayed or inadequate treatment, but this disparity might not be fully reflected in the reported data.
Additionally, racial and ethnic biases within healthcare systems themselves may lead to disparate treatment and care, potentially affecting the outcome of cases.
Factors Affecting Data Accuracy
Several factors can compromise the accuracy of the mortality data. Incomplete or inaccurate information regarding underlying health conditions can misrepresent the true cause of death. Differences in coding practices across healthcare facilities can lead to inconsistencies in diagnosis and classification of causes of death. Furthermore, the potential for underreporting of deaths due to the virus, especially in marginalized communities, could significantly underestimate the true extent of the disparity.
Data Gaps Requiring Further Research
A crucial gap in the data involves the lack of detailed information on specific socioeconomic factors, such as housing conditions, access to healthy food, and employment status. These factors play a vital role in understanding the context surrounding disparities. Furthermore, the data may lack detailed information on access to and utilization of preventative measures, like vaccination rates and mask-wearing practices, within specific communities.
Summary Table of Data Limitations
| Limitation Category | Description | Impact on Analysis |
|---|---|---|
| Data Collection Methods | Inconsistencies in reporting criteria across jurisdictions, potential underreporting in vulnerable populations. | Complicates direct comparisons, obscures true patterns of disparity. |
| Potential Biases | Socioeconomic factors (access to healthcare), racial and ethnic biases within healthcare systems. | May misrepresent true mortality rates in vulnerable populations, leading to inaccurate conclusions. |
| Data Accuracy Factors | Incomplete or inaccurate information on underlying health conditions, differences in coding practices. | Misrepresents true cause of death, leads to inconsistencies in diagnosis. |
| Data Gaps | Lack of detailed socioeconomic data, limited information on access to preventative measures. | Impairs understanding of the context surrounding disparities, underestimates the impact of specific factors. |
Last Word

In conclusion, the disparity in coronavirus case deaths across Black and African American counties underscores the need for comprehensive public health strategies. Addressing systemic inequities in healthcare access, socioeconomic factors, and preventative measures is critical to reducing these disparities. Further research and community engagement are vital to achieving equitable health outcomes.