National Diabetes Month misdiagnosis cgm insulin pump: This month, let’s delve into the complexities of diabetes management, focusing on the critical issue of misdiagnosis and how innovative technologies like continuous glucose monitoring (CGM) and insulin pumps can play a pivotal role in achieving better outcomes. Early detection is paramount, but even with advancements in diagnostics, misdiagnosis remains a challenge.
This month-long exploration will examine the historical context of awareness campaigns, the common pitfalls of misdiagnosis, and the transformative impact of CGM and insulin pumps on personalized diabetes care.
We’ll review the typical symptoms of diabetes, contrasting them with symptoms of other conditions to highlight the potential for misdiagnosis. Moreover, we’ll discuss the benefits and limitations of CGM technology, exploring how it enhances blood glucose monitoring and allows for more precise insulin adjustments using insulin pumps. This discussion will encompass various aspects, from the mechanics of insulin pumps to the role of patient education and support in managing the condition effectively.
National Diabetes Month Awareness Campaigns
National Diabetes Month serves as a crucial platform for raising awareness about diabetes and promoting preventative measures. This dedicated time allows for targeted outreach, education, and support for individuals affected by the condition. Understanding the history, evolution, and methods of these campaigns provides valuable insight into the ongoing efforts to combat diabetes.Diabetes awareness campaigns have evolved significantly over the years, adapting to new research, advancements in treatment, and changing societal needs.
Early campaigns often focused primarily on informing the public about the condition, symptoms, and risk factors. Over time, the messaging has become more nuanced, emphasizing the importance of early diagnosis, healthy lifestyle choices, and ongoing management strategies. This shift reflects a broader understanding of the multifaceted nature of diabetes care.
Historical Overview of Awareness Campaigns
Early National Diabetes Month campaigns primarily focused on educating the public about the disease and its symptoms. Information was disseminated through various channels, including print media, radio broadcasts, and public service announcements. These campaigns often emphasized the importance of early diagnosis and treatment. Early efforts lacked the level of patient-centered care and individualized management strategies that are now integral to effective diabetes management.
Evolution of Messaging and Target Audiences
The evolution of diabetes awareness campaigns has been marked by a shift in messaging and target audiences. Initial campaigns predominantly focused on general public awareness. However, more recent campaigns recognize the importance of tailoring messages to specific populations, such as children, adolescents, and ethnic minorities, who may face unique challenges in managing diabetes. The increased focus on patient-centered care and the promotion of self-management skills reflects a modern understanding of diabetes management.
Typical Methods for Public Outreach
Public outreach during National Diabetes Month typically involves a multi-faceted approach. This includes community events, educational workshops, and partnerships with healthcare providers. Social media platforms play a crucial role in disseminating information and engaging with potential audiences. The use of technology and digital media is an increasingly important component of modern campaigns. This multi-pronged approach ensures that a wide range of people are exposed to crucial information about diabetes.
- Community events: Local fairs, health expos, and screenings are common ways to engage the public and provide direct access to information.
- Educational workshops: Workshops led by medical professionals, dietitians, and diabetes educators provide practical knowledge and hands-on skills.
- Social media campaigns: Utilizing platforms like Facebook, Twitter, and Instagram to reach a broad audience with informative posts, videos, and interactive content.
- Partnerships with healthcare providers: Collaborating with doctors, nurses, and other healthcare professionals allows for the integration of diabetes management into routine care.
Successful Awareness Campaigns, National diabetes month misdiagnosis cgm insulin pump
Numerous campaigns have demonstrated success in raising awareness and impacting diabetes management. For instance, campaigns focusing on early detection and the importance of regular check-ups have significantly improved diagnosis rates. Campaigns highlighting the benefits of a healthy lifestyle have encouraged people to make positive changes to their diet and exercise routines. The long-term impact of these campaigns is often seen in improved health outcomes and reduced complications associated with diabetes.
Hypothetical National Diabetes Month Campaign Focused on Reducing Misdiagnosis Rates
A hypothetical campaign focused on reducing misdiagnosis rates would emphasize the importance of accurate symptom recognition and early diagnosis. It would feature educational materials, online resources, and partnerships with primary care physicians to enhance diagnostic capabilities. The campaign would target healthcare providers, patients, and family members.
Potential Challenges for Executing a Successful Campaign
Executing a successful campaign presents several challenges. Budget constraints can limit the scope and reach of outreach efforts. Ensuring the campaign aligns with existing resources and expertise within the community is crucial for successful implementation. Maintaining public engagement and interest over time is also a key factor. Other challenges may include coordination among various stakeholders and a lack of community awareness.
- Budget constraints: Limited financial resources can restrict the scope and impact of outreach efforts.
- Resource limitations: Ensuring access to qualified healthcare professionals and educational materials in underserved communities can be challenging.
- Maintaining public engagement: Sustaining public interest and participation in awareness campaigns over an extended period requires innovative strategies.
- Coordination among stakeholders: Effective communication and collaboration between government agencies, healthcare providers, and community organizations are essential.
Misdiagnosis of Diabetes
Diabetes, a chronic metabolic disorder, can be challenging to diagnose, especially in its early stages. Misdiagnosis can lead to delayed treatment, potentially serious complications, and a decreased quality of life for individuals affected. Understanding the reasons behind misdiagnosis, recognizing subtle symptoms, and grasping the nuances of diagnostic tests is crucial for both patients and healthcare providers.
Common Reasons for Misdiagnosis
Misdiagnosis of diabetes often stems from a combination of factors. Symptoms might be subtle or masked by other conditions, leading clinicians to overlook the possibility of diabetes. Lack of awareness about the disease’s diverse presentation, especially in its early stages, also contributes. Furthermore, variations in diagnostic criteria and the limitations of specific tests can further complicate accurate diagnosis.
Some patients may also experience inconsistent or fluctuating symptoms, making it difficult to establish a clear pattern. The complex interplay of these factors highlights the importance of meticulous evaluation and thorough investigation.
Symptoms Often Misinterpreted in Early-Stage Diabetes
Early-stage diabetes often presents with vague symptoms that can be easily overlooked or attributed to other conditions. Polyuria (excessive urination), especially at night, and increased thirst are common early indicators. Fatigue and unexplained weight loss are also frequently encountered but can be mistaken for other issues. Blurred vision, recurrent infections, and slow-healing sores can also be subtle signs of diabetes, sometimes not noticed until more advanced stages.
The subtlety of these symptoms emphasizes the importance of routine check-ups and open communication with healthcare professionals.
Diagnostic Tests and Their Limitations
Various diagnostic tests are used to identify diabetes, including fasting plasma glucose (FPG) tests, oral glucose tolerance tests (OGTT), and random plasma glucose (RPG) tests. The fasting plasma glucose test measures blood sugar levels after an overnight fast. The oral glucose tolerance test assesses blood sugar response after consuming a sugary drink. The random plasma glucose test measures blood sugar levels at a random time, regardless of meal timing.
However, each test has limitations. For example, the fasting plasma glucose test may miss individuals with impaired glucose tolerance. Similarly, the oral glucose tolerance test can be influenced by factors like stress or medications. The random plasma glucose test may be unreliable if the individual hasn’t eaten for a significant time before the test. Recognizing these limitations is essential for accurate interpretation and follow-up evaluations.
Comparing Type 1 and Type 2 Diabetes Symptoms
While both type 1 and type 2 diabetes share some common symptoms, crucial differences exist. Type 1 diabetes typically manifests acutely with rapid onset of symptoms such as extreme thirst, frequent urination, and rapid weight loss. Type 2 diabetes, on the other hand, often develops gradually, with symptoms often subtle and easily overlooked. Fatigue, increased hunger, and recurrent infections are more common in the initial stages of type 2 diabetes.
The progressive nature of type 2 diabetes means symptoms can be more subtle and develop over time, leading to delayed diagnosis.
Impact of Misdiagnosis on Patient Management
Misdiagnosis of diabetes significantly impacts patient management. Delayed treatment can lead to serious complications like diabetic neuropathy, nephropathy, and retinopathy. Cardiovascular disease risk also increases substantially in individuals with undiagnosed or poorly managed diabetes. Furthermore, the psychological impact of misdiagnosis can be profound, leading to anxiety, depression, and feelings of isolation. Accurate and timely diagnosis is paramount for effective patient management and reducing long-term complications.
Symptoms Comparison Table
| Symptom | Diabetes | Other Conditions (Examples) |
|---|---|---|
| Excessive Thirst | Common | Dehydration, certain medications |
| Frequent Urination | Common | Urinary tract infections, kidney problems |
| Unexplained Weight Loss | Possible, especially in type 1 | Malnutrition, hyperthyroidism |
| Fatigue | Common | Anemia, depression, sleep disorders |
| Blurred Vision | Possible | Eye strain, cataracts |
Continuous Glucose Monitoring (CGM) Technology
Continuous Glucose Monitoring (CGM) technology has revolutionized diabetes management by providing real-time glucose readings. This continuous feedback loop allows individuals with diabetes to better understand their glucose fluctuations and make more informed decisions about food intake, exercise, and insulin adjustments. This technology is a powerful tool in the fight against diabetes complications and helps improve quality of life.CGM systems work by constantly measuring glucose levels in interstitial fluid, a liquid surrounding the cells.
This information is then transmitted to a receiver, such as a smartphone app or a small handheld device, allowing users to track their glucose trends throughout the day. This data provides valuable insights into how different factors affect glucose levels, which can be extremely helpful in making adjustments to daily routines.
Function and Benefits of CGM Technology
CGM systems continuously monitor glucose levels in the interstitial fluid, providing a more comprehensive picture of glucose fluctuations compared to traditional finger-prick blood glucose monitoring. This continuous data allows for proactive adjustments to treatment plans, potentially reducing the risk of hyperglycemia and hypoglycemia. The ability to track trends over time allows users to better understand how different factors, such as meals, exercise, and stress, impact their glucose levels.
This understanding facilitates personalized strategies for improved glucose control.
Limitations and Potential Complications of CGM Use
While CGM offers significant advantages, it’s important to acknowledge its limitations. Accuracy can vary between devices and individuals, and calibration errors can lead to inaccurate readings. Furthermore, CGM sensors need to be replaced regularly, and skin reactions, such as redness or irritation, can occur at the sensor insertion site. Users should be aware of these potential issues and take steps to mitigate them, such as proper sensor insertion technique and appropriate skin care.
Role of CGM in Improving Diabetes Management
CGM data empowers individuals with diabetes to actively manage their condition. By providing real-time glucose insights, CGM facilitates timely adjustments to insulin doses, meals, and physical activity. This proactive approach reduces the risk of severe hyperglycemia and hypoglycemia, which are major complications associated with diabetes. This improved glucose control can lead to a reduction in long-term health risks.
Adjusting Insulin Doses Using CGM Data
CGM data provides crucial information for insulin dose adjustments. For example, if a CGM reading indicates a rising glucose level, the user can adjust their insulin dose accordingly to prevent hyperglycemia. Conversely, if a reading indicates a dangerously low glucose level, the user can take immediate corrective action to prevent hypoglycemia. These adjustments can be made through various methods, including using a CGM-compatible insulin pump or manual insulin dose adjustments.
The key is to learn how to interpret the CGM data in relation to personal responses to different foods and activities.
Examples of Different CGM Devices and Their Features
Several CGM devices are available, each with unique features. Some devices provide alerts for low or high glucose levels, while others offer detailed trend analysis and data visualization tools. Many devices can integrate with compatible insulin pumps, enabling automated insulin delivery based on real-time glucose data.
Summary Table of CGM Devices
| CGM Device | Key Features |
|---|---|
| Dexcom G6 | Real-time glucose readings, alerts for high/low glucose, trend analysis, integration with insulin pumps |
| FreeStyle Libre 2 | Non-invasive, continuous glucose monitoring, readings without finger pricks, alerts for high/low glucose |
| Eversense | Implantable CGM sensor, providing readings for up to 90 days, advanced data analysis |
Insulin Pump Therapy
Insulin pump therapy is a sophisticated method for managing blood sugar levels in individuals with diabetes. It offers a more flexible and potentially more convenient alternative to traditional insulin injections, allowing for precise and continuous insulin delivery. Understanding the mechanics, advantages, and potential complications is crucial for those considering this treatment option.Insulin pumps are small, computerized devices that deliver insulin subcutaneously (under the skin) through a thin cannula.
National Diabetes Month is a great time to reflect on misdiagnosis and the importance of continuous glucose monitors (CGM) and insulin pumps. While navigating the complexities of diabetes management, it’s also cool to see how creative people are using existing concepts. For example, check out this exciting new take on superhero movies, a sleight trailer for a superhero movie, reimagining Iron Man with a fresh spin sleight trailer superhero movie iron man remix.
Ultimately, though, focusing on the right tools, like CGMs and insulin pumps, can make a real difference in managing diabetes effectively.
The pump is programmed to deliver insulin based on the individual’s needs, determined by factors like carbohydrate intake, physical activity, and blood glucose readings. These devices work by providing a basal rate of insulin (a continuous, low dose) throughout the day and then adjusting based on bolus doses (additional insulin needed) required for meals or to correct high blood sugar levels.
Mechanics of Insulin Pump Therapy
Insulin pumps work by continuously delivering a basal rate of insulin, mimicking the body’s natural insulin production. This continuous delivery ensures a stable blood glucose level. Bolus doses are administered as needed to manage meals and correct high blood sugar readings. Users typically program the pump based on individual needs and preferences, adjusting the basal rate and bolus amounts.
The pump’s computerized system calculates the amount of insulin needed based on the user’s input and settings.
Advantages of Insulin Pump Therapy
Insulin pumps offer several benefits compared to traditional insulin injections. Improved blood glucose control is a key advantage, as the continuous delivery allows for more precise management of blood sugar fluctuations. This precision can lead to reduced episodes of hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). The flexibility of the pump also allows for a more active lifestyle, as users can adjust insulin delivery based on their activity levels.
National Diabetes Month is a great time to reflect on the importance of accurate diagnoses, especially when considering continuous glucose monitors (CGMs) and insulin pumps. While advancements in tech like the Fitbit Charge 3’s release date announced price are exciting ( fitbit charge 3 release date announced price ), it’s crucial to remember that these tools are just one part of a holistic approach to managing diabetes.
Early detection and proper medical guidance remain essential for optimal health outcomes during National Diabetes Month.
It can also enhance the quality of life for individuals with diabetes.
Disadvantages of Insulin Pump Therapy
While insulin pumps offer many advantages, there are potential drawbacks. The initial cost of the pump and supplies can be significant. The responsibility for pump maintenance and accurate programming rests with the user. Users must also manage the risk of potential complications, such as cannula site reactions, infections, and pump malfunction. Continuous monitoring and care are necessary.
Importance of Proper Insulin Pump Training and Maintenance
Thorough training from a qualified healthcare professional is essential for safe and effective insulin pump use. This training should cover programming the pump, administering insulin, recognizing signs of complications, and troubleshooting issues. Regular maintenance, including checking the cannula site for signs of infection or irritation, is critical for preventing complications. Users should also be aware of the importance of proper insulin storage and pump care to ensure its longevity and effectiveness.
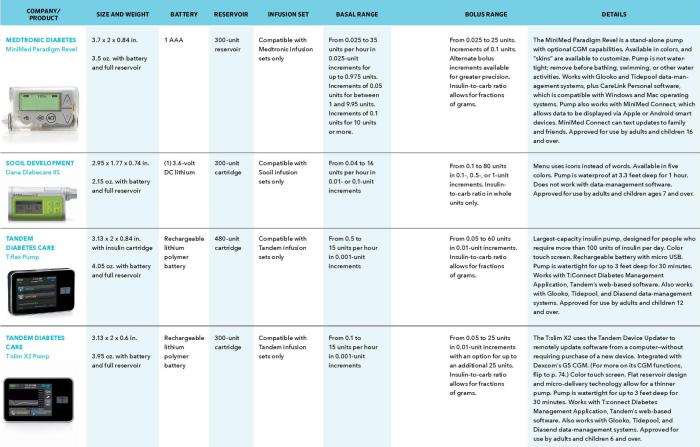
Examples of Different Insulin Pump Types and Features
Different insulin pump models offer varying features and capabilities. Some pumps provide real-time glucose monitoring, allowing users to see their blood glucose levels and adjust insulin delivery accordingly. Others offer more advanced features, like the ability to automatically adjust insulin delivery based on the user’s activity levels or carbohydrate intake. There are also pumps with alarms for low blood sugar or other alerts, promoting user safety.
The choice of pump will depend on individual needs and preferences.
Potential Complications Associated with Insulin Pump Use
Potential complications associated with insulin pump use include cannula site reactions (redness, swelling, or pain), infections at the insertion site, and pump malfunction. The risk of hypoglycemia or hyperglycemia can also be present, but with proper training and monitoring, these risks can be mitigated. Users should be aware of these potential complications and understand how to manage them effectively.
Comparison of Insulin Pump Therapy with Traditional Insulin Injections
Insulin pump therapy differs significantly from traditional insulin injections. Pumps offer continuous insulin delivery, whereas injections require multiple daily doses. Pump therapy provides more flexibility and precise control over blood glucose levels, potentially leading to better management and fewer fluctuations. However, pumps require a higher level of commitment to training, maintenance, and vigilance for potential complications. Users should discuss both options with their healthcare provider to determine the best approach for their individual needs.
Intersection of Misdiagnosis, CGM, and Insulin Pumps
Navigating the complexities of diabetes management often involves a delicate dance between accurate diagnosis, effective treatment, and personalized care. Misdiagnosis can significantly delay appropriate intervention, leading to complications and impacting overall health. Continuous Glucose Monitoring (CGM) and insulin pumps offer powerful tools to enhance diabetes management and potentially prevent misdiagnosis. This intersection of technologies provides a promising avenue for improved outcomes and personalized treatment plans.CGM data, meticulously collected over time, offers a wealth of information about glucose fluctuations.
This data can be a crucial factor in identifying patterns and trends that might otherwise be missed, helping to differentiate between pre-diabetes, impaired glucose tolerance, and actual diabetes. This detailed data helps refine diagnoses and adjust treatment strategies.
CGM Data in Preventing Misdiagnosis
CGM technology provides a comprehensive, real-time view of blood glucose levels, offering crucial insights into the dynamic nature of blood sugar fluctuations. This data can be analyzed to identify trends and patterns that might not be apparent from infrequent or inaccurate traditional blood sugar checks. For example, a patient experiencing seemingly normal fasting blood sugar but exhibiting consistently elevated glucose levels after meals might be identified as having a misdiagnosis if the patient is only relying on fasting blood sugar readings.
CGM data can help identify this pattern and indicate a need for further evaluation, potentially leading to a more accurate diagnosis.
Insulin Pumps in Managing Blood Glucose After Accurate Diagnosis
Insulin pumps, coupled with an accurate diagnosis, offer a precise and personalized approach to managing blood glucose levels. They allow for flexible and tailored insulin delivery, accommodating the unique needs of each individual. This precise control can help patients achieve and maintain optimal blood glucose levels, reducing the risk of complications associated with poorly managed diabetes. By delivering insulin on demand, or based on a pre-programmed basal rate, the pump minimizes fluctuations and helps in achieving target glucose levels.
CGM and Insulin Pumps for Personalized Treatment Plans
The combination of CGM and insulin pumps empowers healthcare providers to create highly personalized treatment plans. CGM data provides real-time information about glucose responses to meals, exercise, and other factors. This information can be integrated with insulin pump settings, enabling adjustments in insulin delivery based on individual needs. For example, a patient using CGM might notice a consistent pattern of higher glucose spikes after consuming sugary drinks.
This data can be used to adjust the insulin pump’s bolus dose for those specific meals, ensuring a more effective and personalized response.
Improved Outcomes with CGM and Insulin Pumps
Using both CGM and insulin pumps can lead to a significant improvement in overall patient outcomes. Reduced fluctuations in blood glucose levels contribute to better long-term health, reducing the risk of chronic complications such as neuropathy, nephropathy, and retinopathy. The ability to proactively manage blood glucose levels can positively impact quality of life and reduce the burden of diabetes management.
This personalized approach allows for a more active role in self-management, leading to improved patient satisfaction and engagement in their care.
Benefits and Challenges of Integrating CGM and Insulin Pumps
| Benefits | Challenges |
|---|---|
| Improved glucose control | Cost of the technology |
| Reduced risk of complications | Potential for technical difficulties |
| Personalized treatment plans | Requires significant training and education |
| Enhanced patient empowerment | Potential for data overload and interpretation |
| Increased adherence to treatment | Need for ongoing support and maintenance |
Patient Education and Support
Navigating a diabetes diagnosis can be overwhelming. Understanding the condition, managing it effectively, and accessing support are crucial for positive outcomes. This section focuses on the vital role of patient education and support in the journey of living with diabetes, including misdiagnosis scenarios and the use of advanced technologies like CGM and insulin pumps.Effective diabetes management hinges on comprehensive patient education.
National Diabetes Month is a great time to talk about misdiagnosis and the importance of continuous glucose monitors (CGMs) and insulin pumps. While advancements in these technologies are helping people better manage their diabetes, it’s important to remember that the internet plays a crucial role in patient education and support, like this recent approval of the Net Neutrality Save the Internet Act in the House of Representatives.
This legislation will help ensure patients have access to accurate and up-to-date information, ultimately aiding in preventing misdiagnosis and improving diabetes management outcomes. This support is crucial for those navigating the complexities of diabetes care.
Knowledge empowers individuals to make informed decisions about their health, leading to better control of blood glucose levels and improved overall well-being. It’s a cornerstone of successful diabetes management.
Resources for Patients Facing Misdiagnosis
Numerous resources are available to assist patients who suspect a misdiagnosis. These resources provide information about the symptoms of diabetes, potential diagnostic errors, and the importance of seeking a second opinion. Patient advocacy groups, medical professionals, and online platforms can offer valuable guidance.
- Patient Advocacy Groups: Organizations like the American Diabetes Association (ADA) and the Juvenile Diabetes Research Foundation (JDRF) provide educational materials, support groups, and information about the latest research and treatment options. They often have dedicated sections on the challenges of misdiagnosis and support for those who suspect they may have been misdiagnosed.
- Medical Professionals: Consulting with endocrinologists, diabetologists, or other qualified healthcare providers can provide crucial insights and a thorough evaluation of the individual’s situation. A second opinion is highly recommended, especially if there are concerns about the initial diagnosis.
- Online Platforms: Online forums and support groups offer a space for patients to share experiences, ask questions, and connect with others facing similar challenges. These communities can provide valuable insights and support.
Importance of Patient Education on Diabetes Self-Management
Diabetes self-management education is critical for effectively controlling blood glucose levels and preventing complications. It equips patients with the knowledge and skills to monitor their condition, adjust their treatment plan as needed, and make healthy lifestyle choices.
- Understanding Blood Glucose Monitoring: Proper technique for using glucose meters and interpreting results is essential. Learning to recognize patterns in blood glucose levels and identify triggers for fluctuations is key to effective management.
- Nutritional Guidance: Developing a personalized meal plan that aligns with individual needs and preferences is critical. This involves understanding carbohydrate counting, portion control, and making healthy food choices. Nutritional counseling can provide personalized dietary advice.
- Exercise and Physical Activity: Incorporating regular physical activity into daily routines is essential for managing blood glucose levels. Educating patients about the impact of exercise on blood sugar and appropriate exercise routines is vital.
- Medication Management: Understanding the purpose, dosage, and potential side effects of diabetes medications is crucial. Proper administration and adherence to the prescribed treatment plan are essential.
Role of Support Groups and Online Communities
Support groups and online communities play a vital role in the emotional and practical well-being of people living with diabetes. These spaces offer a safe environment to share experiences, receive encouragement, and connect with others who understand the challenges.
- Emotional Support: Diabetes can be emotionally challenging. Support groups provide a safe space for individuals to express their feelings, anxieties, and concerns. They allow for the sharing of experiences and coping mechanisms.
- Practical Advice and Tips: Members of support groups often share valuable practical tips and advice on managing diabetes effectively. This includes information on meal planning, exercise routines, and medication management.
- Connection with Others: Connecting with other individuals with similar experiences creates a sense of community and belonging. This can be especially beneficial during challenging times.
Organizations Offering Support for Patients
Numerous organizations offer support and resources for patients with diabetes. These organizations often provide educational materials, support groups, and other services tailored to the specific needs of individuals living with the condition.
- American Diabetes Association (ADA): A leading organization providing resources, support, and advocacy for people with diabetes.
- Juvenile Diabetes Research Foundation (JDRF): Focused on research and funding for type 1 diabetes.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): A government agency dedicated to research, education, and support for diabetes and related conditions.
- The Endocrine Society: A professional organization for endocrinologists, offering information and resources for patients.
Using CGM Data to Manage Insulin Pump Settings
Continuous Glucose Monitoring (CGM) data provides real-time insights into blood glucose levels, enabling users to fine-tune their insulin pump settings for optimal glucose control.
| CGM Reading | Insulin Pump Adjustment |
|---|---|
| High Glucose | Adjust insulin dose based on CGM trend. Increase basal rate or adjust bolus amount accordingly. |
| Low Glucose | Reduce basal rate and/or administer a corrective bolus. |
| Stable Glucose | Maintain current insulin pump settings. |
Impact of Misdiagnosis on Healthcare System: National Diabetes Month Misdiagnosis Cgm Insulin Pump
Misdiagnosis of diabetes, while seemingly a personal health concern, significantly impacts the healthcare system as a whole. The financial burden on individuals and the broader system is substantial, compounded by the long-term health complications that arise from delayed or inaccurate diagnoses. This ripple effect underscores the crucial need for improved diagnostic processes and increased patient education.The misdiagnosis of diabetes can lead to a cascade of negative consequences, from unnecessary medical interventions to the development of severe complications.
Addressing these systemic issues requires a multifaceted approach that emphasizes early detection, accurate diagnostic tools, and comprehensive patient support. A focus on these areas can reduce the burden on the healthcare system while improving patient outcomes.
Economic Burden of Misdiagnosis
The economic consequences of diabetes misdiagnosis are multifaceted. Unnecessary treatments, tests, and hospitalizations consume considerable resources. For example, patients misdiagnosed with conditions like anxiety or depression might receive therapies that are ineffective and do not address the underlying diabetes. This leads to a waste of healthcare dollars that could be better allocated to effective treatments. The cost of managing long-term complications associated with undiagnosed diabetes, such as heart disease, kidney failure, and nerve damage, is astronomical.
These long-term consequences often require extensive, expensive care, further straining healthcare budgets.
Long-Term Health Complications
Delayed or incorrect diabetes diagnosis can result in significant long-term health complications. Uncontrolled blood sugar levels damage blood vessels, leading to a range of serious health issues. These include cardiovascular diseases, such as heart attack and stroke, which often lead to hospitalizations and prolonged recovery periods. Furthermore, diabetic nephropathy (kidney disease) and neuropathy (nerve damage) can significantly reduce quality of life and require ongoing medical interventions.
Moreover, retinopathy, or damage to the retina, can lead to vision loss.
Strategies for Reducing Misdiagnosis Rates
Improving diagnostic accuracy requires a multifaceted approach that involves healthcare providers, patients, and researchers. Enhanced training for healthcare professionals on the latest diagnostic criteria and symptoms is crucial. For instance, providing continuing medical education (CME) courses that emphasize the importance of thorough patient history taking and physical examination, particularly in at-risk populations, is vital. Regular audits of diagnostic practices can identify and address potential errors in diagnosis.
Improved access to advanced diagnostic tools, such as continuous glucose monitoring (CGM) devices, can aid in earlier and more accurate diagnosis, especially in cases of suspected but uncertain diabetes.
Importance of Early Diagnosis in Diabetes Management
Early diagnosis of diabetes is critical for effective management and preventing serious complications. The earlier the disease is detected, the sooner treatment can begin. This allows for proactive lifestyle changes, medication adjustments, and consistent monitoring, all contributing to better blood sugar control and reduced risk of long-term complications. The benefits of early intervention extend to improved quality of life and reduced healthcare costs.
Recommendations to Improve the Accuracy of Diabetes Diagnoses
Improving the accuracy of diabetes diagnoses necessitates a collaborative effort among all stakeholders. The following recommendations are crucial:
- Comprehensive Patient History: Thorough questioning about symptoms, family history, and lifestyle factors can significantly aid in accurate diagnosis. This includes detailed questioning about symptoms that might be overlooked, like frequent urination or unexplained weight loss.
- Standardized Diagnostic Criteria: Clear, standardized diagnostic criteria should be readily available and followed consistently across healthcare settings. This reduces variability in diagnosis and ensures that all patients are assessed using the same benchmark.
- Improved Diagnostic Tools: Investing in and utilizing advanced diagnostic tools, such as CGM, can enhance the precision and speed of diagnosis.
- Increased Awareness and Education: Raising public awareness about diabetes symptoms and encouraging early testing is essential for timely intervention.
- Collaboration between Specialists: Promoting communication and collaboration among different healthcare professionals, such as primary care physicians, endocrinologists, and diabetes educators, can improve diagnostic accuracy.
Final Wrap-Up

In conclusion, National Diabetes Month presents a valuable opportunity to raise awareness about the importance of accurate diagnosis and the transformative potential of CGM and insulin pumps. While challenges remain, the integration of these technologies offers a pathway to improved patient outcomes. By understanding the intricacies of misdiagnosis, and the benefits of personalized treatment strategies, we can work toward a future where individuals with diabetes receive the care they deserve.
This month, let’s champion early detection, empower patients, and support a healthier future for those living with diabetes.